
Polycystic Ovary Syndrome (PCOS) is a complex hormonal disorder that affects a significant number of women worldwide. While the exact causes of PCOS are not fully understood, research has established a strong link between PCOS and obesity. This relationship is intricate, with each condition exacerbating the other. In this blog, we'll delve into what PCOS is, explore its symptoms and treatment options, and uncover how it's related to obesity.
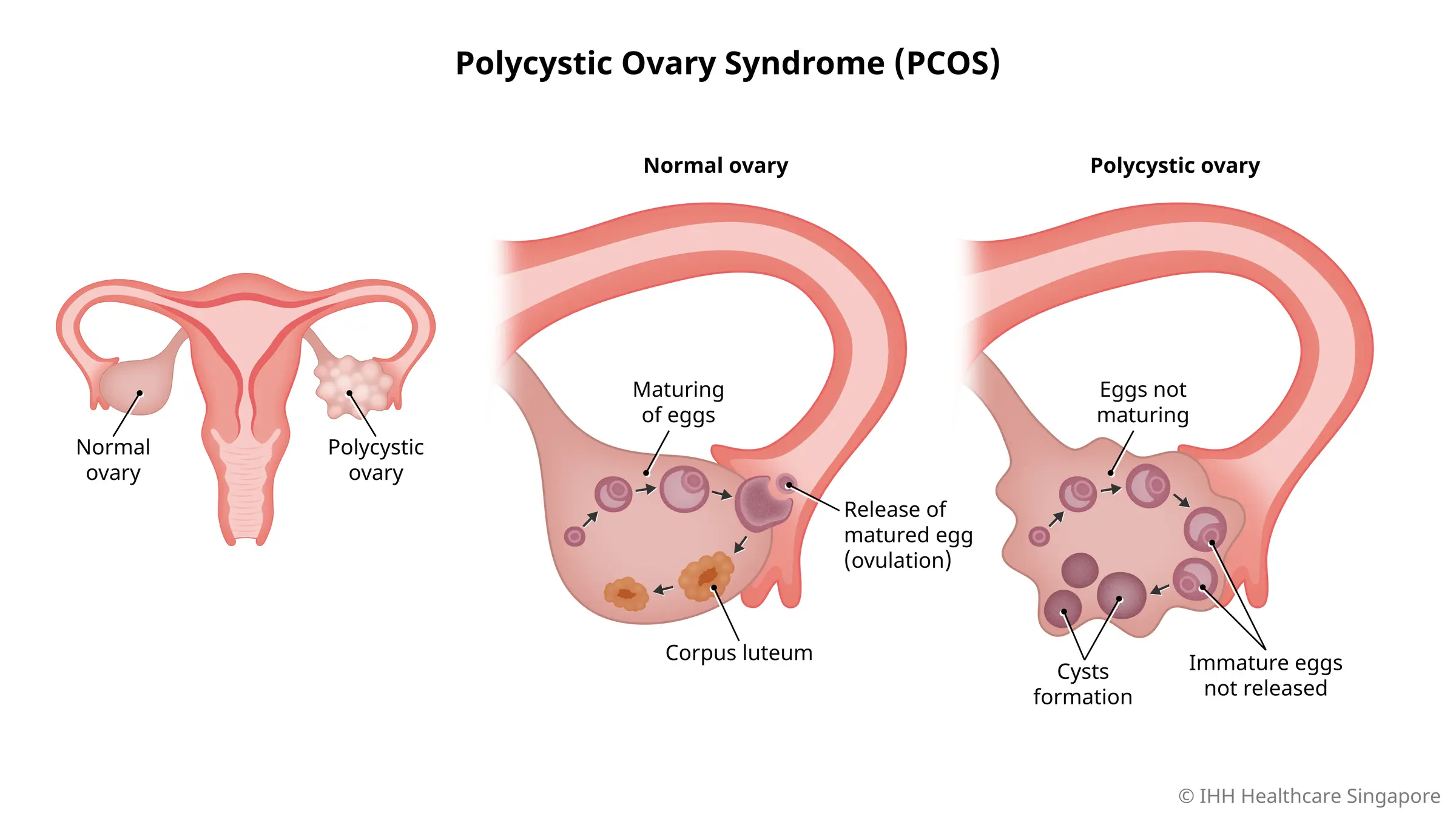
PCOS, or Polycystic Ovary Syndrome, is a multifaceted hormonal condition. The term "polycystic" means "many cysts," referring to the numerous partially developed follicles on the ovaries, each containing an egg. These follicles rarely mature enough to release eggs that can be fertilized.
Women with PCOS typically exhibit high levels of insulin or androgens (male hormones), or both. The underlying cause remains unclear, but insulin resistance is believed to be a significant driving factor of this syndrome. PCOS can occur in families or manifest when a woman gains weight.
PCOS is relatively prevalent, especially among women experiencing infertility, affecting 12 to 18 percent of women of reproductive age, from late adolescence to menopause. Surprisingly, nearly 70 percent of cases remain undiagnosed. It's worth noting that up to a third of women may have polycystic ovaries visible on an ultrasound, but not all will have PCOS. Diagnosis usually hinges on the presence of polycystic ovaries or typical symptoms of the syndrome.
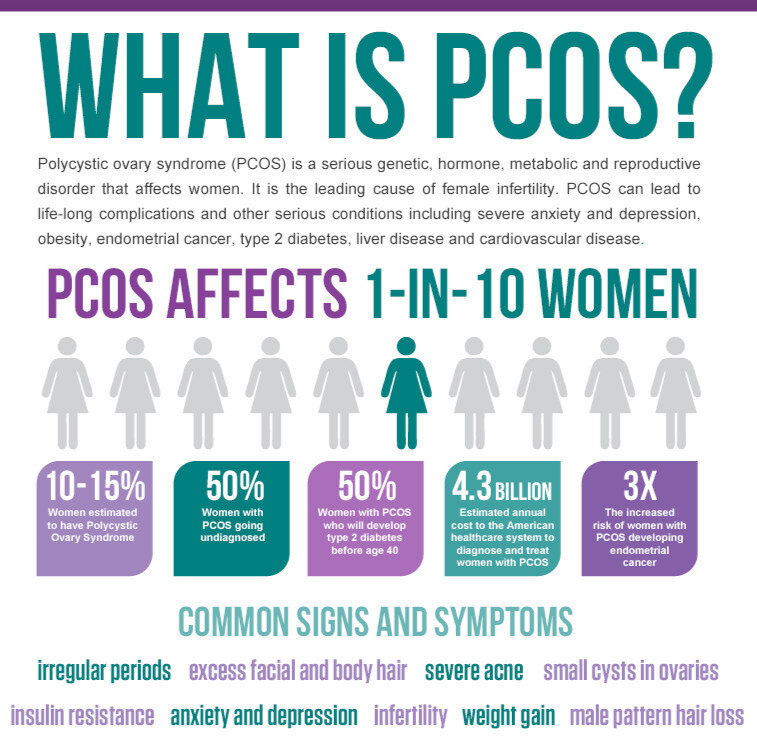
Women affected by PCOS might experience a variety of symptoms, including:
It's important to note that not all women with PCOS will exhibit all these symptoms.
The relationship between PCOS and obesity is bidirectional and complex:
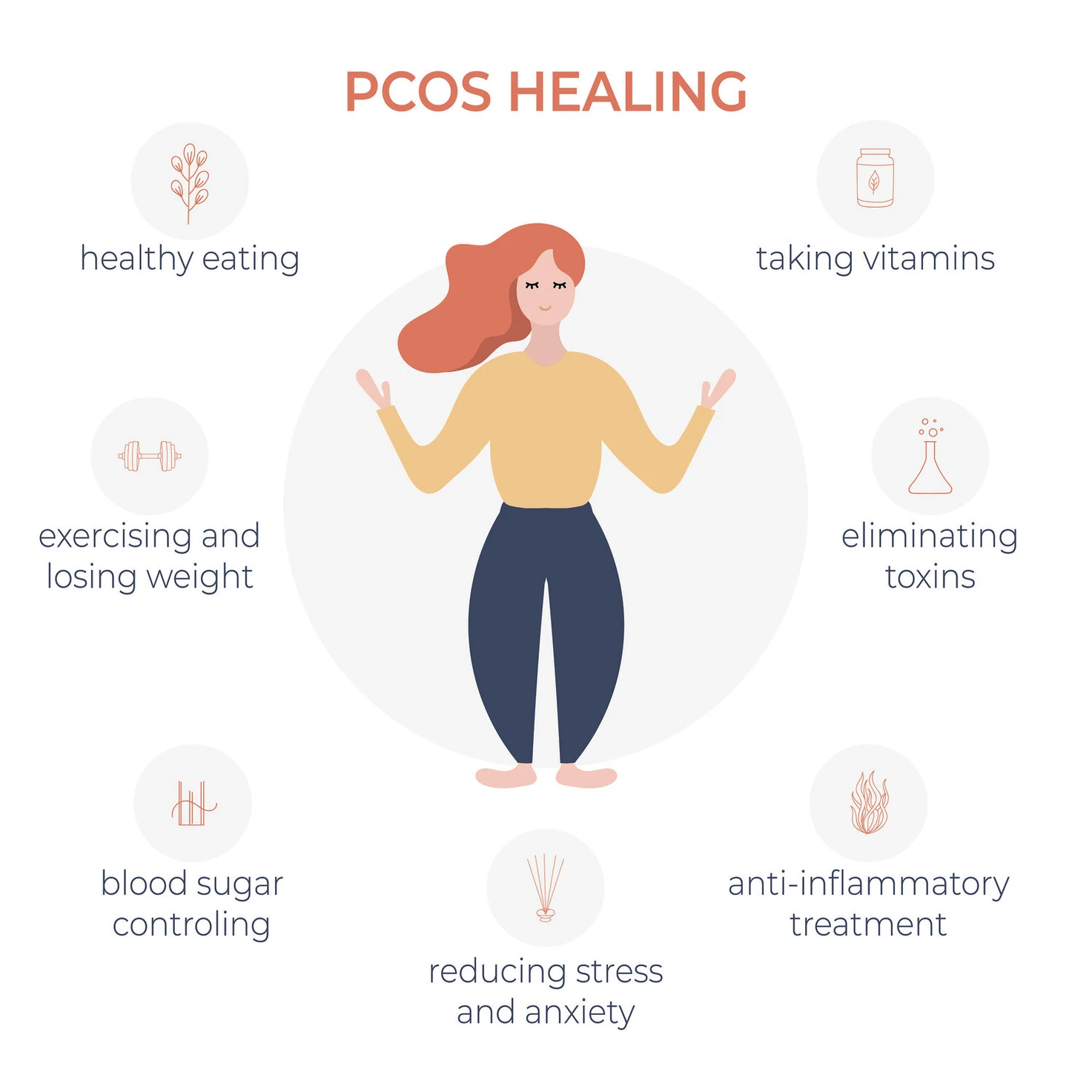
Effectively managing PCOS requires a comprehensive approach that includes lifestyle modifications, medical interventions, and professional guidance:
Lifestyle Modifications :
Weight Reduction :
Medical Treatment :
Professional Guidance :

PCOS is associated with several long-term health risks, including:
Early diagnosis of PCOS is crucial for effective management and prevention of long-term complications. Diagnosis typically involves a combination of medical history, physical examination, ultrasound, and blood tests to measure hormone levels.
If you suspect you have PCOS or are struggling with obesity, seek professional medical advice. Healthcare providers that can assist include:
While the interplay between PCOS and obesity is intricate, understanding and managing both conditions can lead to significant health improvements. Lifestyle changes, medical interventions, and comprehensive care can help alleviate symptoms and improve quality of life. Don't hesitate to seek professional assistance for an accurate diagnosis and tailored management plan.
If you are considering weight loss surgery, bariatric surgery, robotic surgery, or need the best hernia surgeon in Hyderabad, look no further than Dr. Abhishek Katakwar at AIG Hospital. Take the first step towards a healthier, happier you by scheduling a consultation today.
Connect with Dr. Katakwar and AIG Hospitals:
© 2026 Dr. Abhishek Katakwar. All Rights Reserved.