
A hernia occurs when an internal organ or tissue pushes through a weak spot in the surrounding muscle or connective tissue. It may cause swelling, pain, or a visible bulge, especially during activities like lifting heavy objects or coughing.
If left untreated, a hernia can lead to serious complications. Timely surgical intervention ensures long-term relief and prevents further issues.

 e-TEP access :
Currently the most advanced and established laparoscopic hernia surgery in the surgical
world. A
highly evolved
procedure that recreates and reinforces the entire weakened abdominal wall via
laparoscopy. The mesh
here is put beneath
the rectus muscle which gives the best favourable outcome. Low pain, faster recovery,
early
discharge are a given here!
e-TEP access :
Currently the most advanced and established laparoscopic hernia surgery in the surgical
world. A
highly evolved
procedure that recreates and reinforces the entire weakened abdominal wall via
laparoscopy. The mesh
here is put beneath
the rectus muscle which gives the best favourable outcome. Low pain, faster recovery,
early
discharge are a given here!
 TAR :
Complex, massive or giant hernia needs specialised procedure for creating extra
abdominal space and
leverage it for
proper closure and wide mesh placement. This is a highly advanced procedure best
performed by an
expert team for such
demanding hernia.
TAR :
Complex, massive or giant hernia needs specialised procedure for creating extra
abdominal space and
leverage it for
proper closure and wide mesh placement. This is a highly advanced procedure best
performed by an
expert team for such
demanding hernia.
 SCOLA :
The Subcutaneous Onlay Laparoscopic Approach is a minimally invasive laparoscopic
surgery for small
umbilical and
Epigastric hernia with distasis recti. For the right patient, this surgery can also be
used to
correct the diastasis of
recti without having to undergo open abdominoplasty.
SCOLA :
The Subcutaneous Onlay Laparoscopic Approach is a minimally invasive laparoscopic
surgery for small
umbilical and
Epigastric hernia with distasis recti. For the right patient, this surgery can also be
used to
correct the diastasis of
recti without having to undergo open abdominoplasty.
 BOTOX :
Hernia with loss of domain needs these extra adjuncts for temporary paralysis of
abdominal muscles.
This helps in
creating the right space inside the abdomen while avoiding some dreaded complications.
BOTOX :
Hernia with loss of domain needs these extra adjuncts for temporary paralysis of
abdominal muscles.
This helps in
creating the right space inside the abdomen while avoiding some dreaded complications.
 PPP :
Preopertive progressive pneumoperitoneum is also an adjunct used in modern hernia
surgery for
creating extra space
inside the abdominal cavity. Used only for loss of domain hernia cases.
PPP :
Preopertive progressive pneumoperitoneum is also an adjunct used in modern hernia
surgery for
creating extra space
inside the abdominal cavity. Used only for loss of domain hernia cases.
 Groin pain :
Groin is the area that connects your lower abdomen to your thighs. An aching groin can
have many
causes like a hidden
groin hernia, hip diseases, lumbar spine diseases, muscle and fascia related pain.
Detailed clinical
history and
clinical examination can point towards the exact cause and the treatment, thereafter.
Groin pain :
Groin is the area that connects your lower abdomen to your thighs. An aching groin can
have many
causes like a hidden
groin hernia, hip diseases, lumbar spine diseases, muscle and fascia related pain.
Detailed clinical
history and
clinical examination can point towards the exact cause and the treatment, thereafter.
 Post operative Chronic groin pain :
Pain after open inguinal hernia surgery can be devastating for patients. But the good
part is it is
treatable. Advanced
knowledge and skills of an abdominal wall reconstruction surgeon lets him correctly
diagnose the
cause and offer the
right treatment for such patients in pain.
Post operative Chronic groin pain :
Pain after open inguinal hernia surgery can be devastating for patients. But the good
part is it is
treatable. Advanced
knowledge and skills of an abdominal wall reconstruction surgeon lets him correctly
diagnose the
cause and offer the
right treatment for such patients in pain.
 Mesh related complications :
Mesh infections are difficult to handle. This needs dedicated team for proper evaluation
and decision
making. The scope
of modern hernia surgery helps in this unfortunate event too.F
Mesh related complications :
Mesh infections are difficult to handle. This needs dedicated team for proper evaluation
and decision
making. The scope
of modern hernia surgery helps in this unfortunate event too.F
Surgical options for hernia repair vary depending on the type and severity of the hernia. Laparoscopic hernia surgery is a minimally invasive technique that involves small incisions, resulting in faster recovery, less pain, and minimal scarring. Open hernia repair is often recommended for larger or more complicated hernias; it involves a short hospital stay and is a highly effective and widely used method. In certain cases, robotic-assisted surgery may be available, offering enhanced precision and control, making it an ideal choice for complex or recurrent hernias.
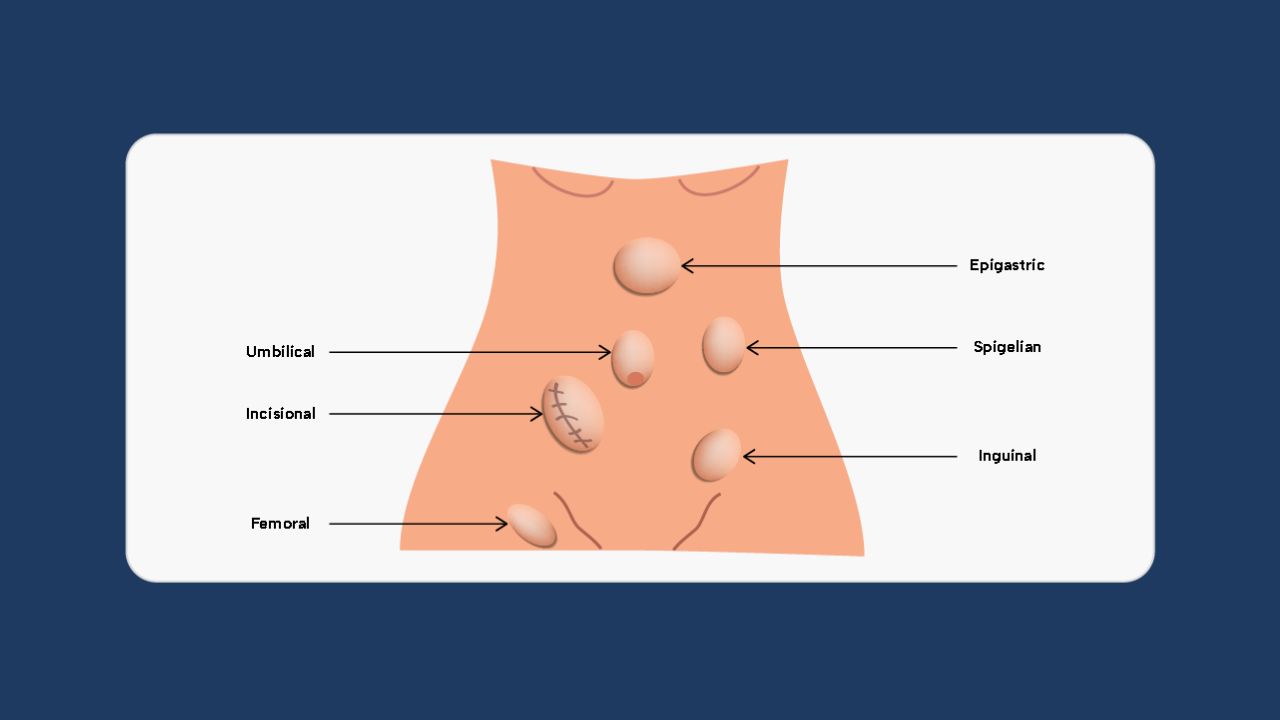
Hernias are broadly categorised as External, which is apparent/visible to the eyes and Internal, which isn’t apparent/visible to the eyes. External hernias, the more common type you hear about, are of several types that are treated by laparoscopy:

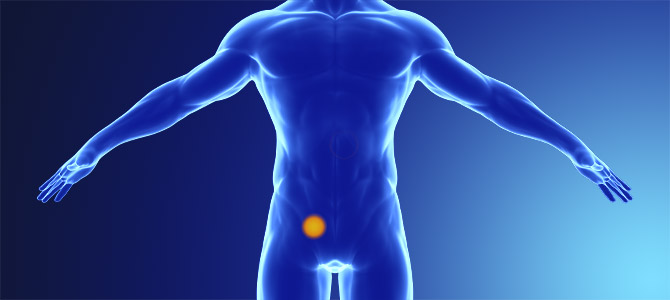
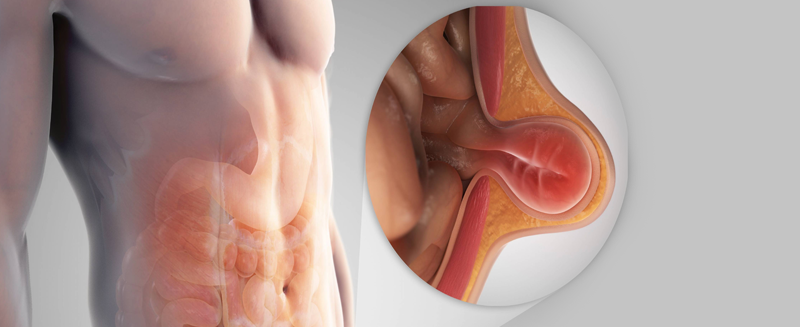
The most commonly heard hernia is an inguinal one. A swelling in the groin which appears on standing, coughing or lifting heavy objects and disappears on lying down is suggestive of an inguinal hernia.
Your umbilicus is the weakest area of your abdominal wall. A bulge in and around the belly button is likely an umbilical hernia. It is very common in females after childbirth due to the stretch of the weakened area. The disfigurement gives an odd look to the umbilicus.

A hernia that appears in the scar of the previous open surgery, less likely laparoscopic surgery, is called an Incisional hernia. If your scar is bulging and your belly looks out of shape after surgery you must see your hernia surgeon immediately. A hernia after a c-section is one such example.

An abdominal wall hernia is a condition where internal organs or fat push through a weakened area in the abdominal muscles, forming a noticeable bulge under the skin.

Another hernia appears in the groin area and is seen more commonly in females than males. These herniae are hard to differentiate from an inguinal hernia, don’t worry leave that to your hernia surgeon!
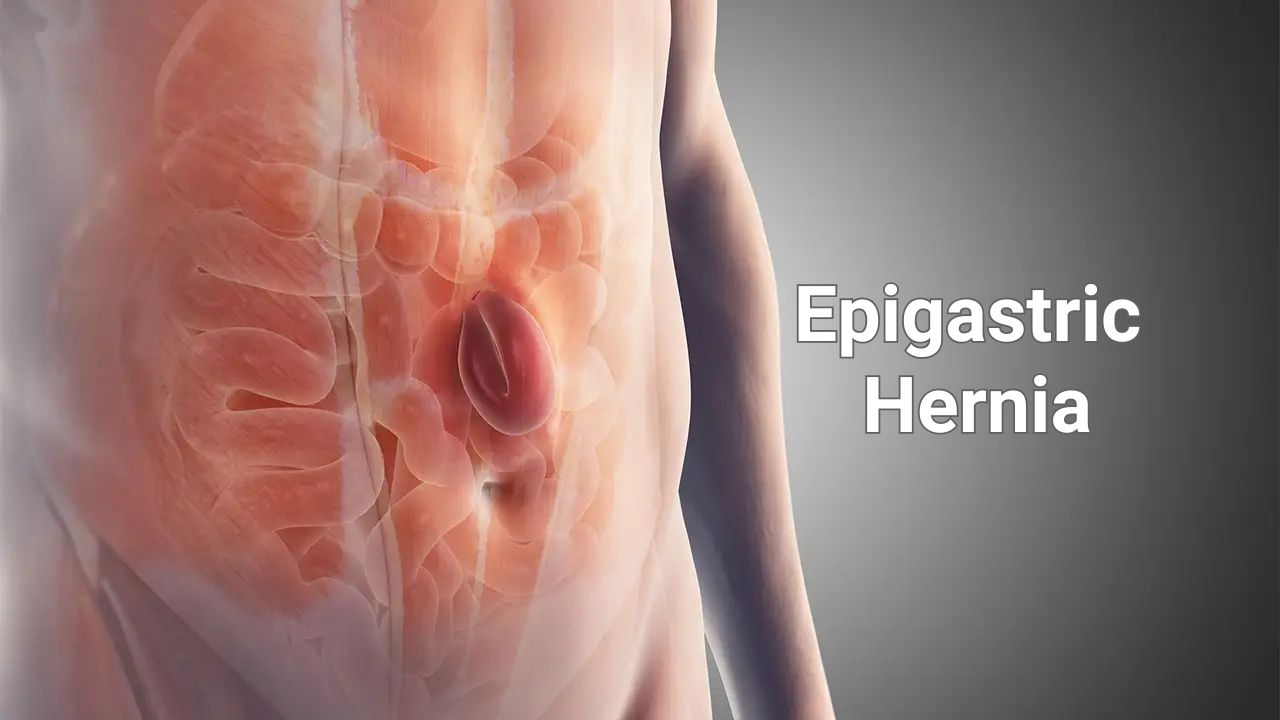
This hernia is in the upper mid abdomen. At times this hernia is hidden. With no apparent swelling and excruciating pain, the diagnosis is often difficult to make. Don’t worry, your hernia surgeon knows exactly how to find them!

Diaphragm is a muscular and partly fascial partition between the chest and abdominal cavity. It helps in maintaining the domain of organs in the respective cavity. A natural gap exists in the diaphragm that allows the oesophagus to pass across from the chest to the abdominal cavity. If this gap increases in size the oesophagus along with the stomach can migrate into the chest cavity. This gives rise to acidity, heartburn, reflux, night cough and even a change of voice.
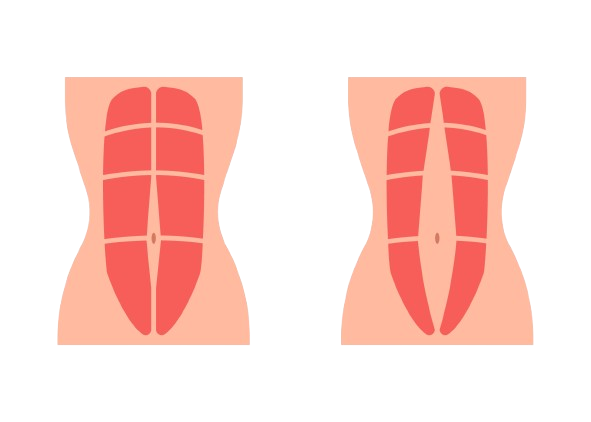
The odd-looking flabby abdomen after childbirth is the result of the separation of the rectus abdominis also known as the six packs muscle. In about 45% of the female, the laxity remains and a banana-shaped swelling appears on straining. This affects the dynamic function of the abdominal wall and puts heavy pressure on the back leading to abnormal posture and backache.

A hernia occurring around the stoma, either urostomy or colostomy, is a parastomal hernia. It affects the function of the stoma due to the pressure effect. This is one of the most complex hernias and requires an abdominal wall reconstruction aka specialist Hernia surgeon. Often these may be associated with an Incisional hernia.
A swelling in the outer part of your abdomen or lower back may be a flank or lumbar hernia. Although rare, these hernia demands special attention and care.
A hernia may be a congenital one or a weakness that occurs post-abdominal surgery. A congenital hernia may present late in adulthood. Irrespective of the cause the treatment options remain the same for adults and laparoscopic hernia surgery is the answer for most.
Prevention is better than cure and it stands right for hernia, too. The content of a hernia can occasionally get obstructed leading to excruciating abdominal pain, vomiting and obstipation. Prolonged obstruction can lead to loss of blood supply to the intestine or omentum. This is a medical emergency which needs attention immediately. Laparoscopic hernia surgery is possible but such emergencies may take away the opportunity of performing laparoscopy due to limited visibility inside the distended abdomen.
Hernia is one of the few diseases that are only treated by surgical correction of the defect and reinforcing the abdominal wall weakness with or without the mesh. Don’t fall prey to hernia drops or any such decoctions as they will never help to close the gap!
The thought of long cuts, poor-looking scars, pain after surgery and delayed recovery is completely mitigated by the highly advanced laparoscopic hernia surgery procedures.
© 2026 Dr. Abhishek Katakwar. All Rights Reserved.